How providers and vendors can stop patient portals from collecting dust
Most healthcare providers taking part in the federal EHR incentive programs give their patients access to their data – but fewer than 33 percent of patients actually take advantage of it, a recent report from the U.S. Government Accountability Office showed.
Patients polled for the study said portals took too much time and effort it took to set up, complained about confusing interface design and said it was a challenge to juggle passwords for several different websites hosted by the places they get care.
So what can the providers who deploy the portals and the vendors who make them do better? Lots, says Jan Oldenburg, founder of Participatory Health Consulting and editor of the recent HIMSS book, Participatory Healthcare: A Person-Centered Approach to Healthcare Transformation.
[Also: GAO finds further proof patients are fed up with portals, EHRs]
"We've known for an awful long time that patients are deeply frustrated with 'multi-portalitis,'" says Oldenburg. "If we were writing meaningful use regs today, we would pay much more attention to common data and helping people get access to a longitudinal record, rather than focusing on each provider doing an independent record of patient care."
That's not just not good for patient access, of course, it's good for enabling better care coordination across provider settings.
"Within communities, clearly physicians vendors, hospitals need to figure out how to join together their data, even if it means they have to give up a little bit of autonomy," said Oldenburg. "They have to figure out how to build common data sources so patients can go to whichever portal they're most comfortable with and see all their data."
There are various ways of doing that, but better leveraging the myriad local, state and national health information exchanges could be a big one.
"That means joining the HIEs, it means pulling HIE data into their EHRs so patients can see their data in one place and physicians can see all of the patient's record," she said. "It makes good sense. Most providers have some sort of HIE, or some type of access to community data. It's past time to figure out how to use that."
The challenge, however, is that it's more or less up to the providers themselves, these days, to encourage each other to do that. The incentives of meaningful use have largely been exhausted, and the future direction of federal requirements isn't exactly crystal clear (evidenced, in part, by an president and a House of Representatives that would like to trim the budget for ONC by a drastic $22 million).
So with the government's power to incentivize vastly reduced, and the onus for better data sharing left to the providers themselves, how confident is Oldenburg that it will happen?
"Depressingly not so much," she said.
"I have been out and about recently and have been having these depressing conversations with hospitals that say 'Oh, yeah, we contribute to the HIE but we don't pull their data in.' Or, 'We make it possible for our providers to see HIE, but it's a hassle and I don't think they do that very much.' Or, 'Our vendor provides for this common database, but I don't think anyone's providing data into it yet – we're sharing that, but we're not seeing much out of it.'"
Still, all it takes is a few bold moves to bring some significant momentum, said Oldenburg.
"It's like telephones or fax machines: There's this tipping point moment where value is created by critical mass, right? Where there's enough data in there that it's like, 'Eureka!' That, suddenly it's worth checking.
"We're not there yet," she added. "I don't honestly know whether the model is going to be that everybody puts their data in HIEs, so the value come from checking the HIE. Or whether everybody starts pulling HIE data into their own repository and so you end up having community data available within your own system. But we're at the cusp of this tipping point, and you can start to imagine you might be almost there."
To help us get there, it could move the needle in a not-insignificant way if patients continue to find their voice – making noise about getting easier and more intuitive access to their longitudinal health data.
"We do know that it makes a difference when patients say to providers, 'This is matters to me, and I'm going to go find someone who's doing this if you're not going to,'" said Oldenburg. "But I worry about the rural and underserved areas where people are less savvy or perhaps don't know what to ask for, or what's possible. If those of us in more connected areas are pushing for it, it's going to make it more of a habit and will start to push the envelope on it.
Vendors also have work to do
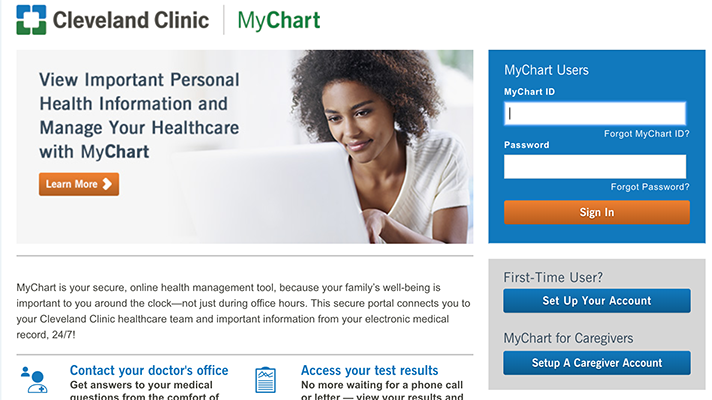
In the meantime, developers of patient portal technology have their work cut out for them as well, she said, starting with something that, in the age of ubiquitous and personalized consumer technology should be a given: simple, elegant, attractive and intuitive user experience.
"If you look at the GAO report you will see that there is significant difference between the rates of adoption across differing vendors," said Oldenburg. "That seems to me to point to the fact that clearly some of the vendors are doing a much better job at UI than others.
"That seems to me to say, 'Gee, guys, you can learn from one another,'" she added. "I don't know whether there is a way for vendors to get an unblinded version of their own information, but if you can it would be well worth looking at it – and figuring out what you're doing less well or more well, and doing more of what other people do well. Clearly, user interface does matter."
Another area for substantial – perhaps fundamental – improvement is a rethinking about just what the existing generation of portals is offering to patients, said Oldenburg.
"The other thing I saw in that GAO data, and I heard from patients as well, is that we've got to get a lot more creative about the features that we offer," she said. "You saw in that survey people saying 'I don't need to go to my portal. I only go around a visit. I go for the features that are useful, or to help me schedule appointments."
In the 21st Century, digital tools are used in nearly every aspect of our lives. Portals could learn some valuable lessons from websites such as Amazon – to pick one example, based only on the fact that its founder this past week became, for a moment at least, the wealthiest man in the world.
"Look at the ways people have gotten creative with online banking and shopping – anticipating the needs we might have, offering suggestions based on analytics about what we've done in the past and our patterns of behavior," said Oldenburg. "We could be doing that for health."
Instead of just logging in once in a while to check lab results, schedule visits and get prescription refills, patient portals could "be much more effective in what we offer and how we offer it and how we make it convenient – going beyond that to anticipate the fact that we might be do for an appointment, or offering suggestions, or thinking about what behavior might be healthy and suggesting things, such as considering the way we walk, the route we take to work and offering suggestions for us," she said.
"I think there are a lot of ways we could learn lessons from the creative digital approaches in other industries," said Oldenburg. "Both in the efficiencies that save money for the systems and time for us, but also nudge us into healthier behaviors."
Twitter: @MikeMiliardHITN
Email the writer: mike.miliard@himssmedia.com























